What is your future with Parkinson's?
No one can accurately predict how your disease will progress - other than it will not get better. People experience diseases differently and respond to medicines differently.
Conversely, in a large group we can predict with more certainty how people with Parkinson's will experience the disease. By understanding these averages, you can make decisions about your medical care and your life.
The most reliable source for those averages are the results seen in placebo-controlled, randomized, blinded clinical trials, in which the people enrolled are randomly chosen to receive the drug or a placebo, and neither they nor their doctor knows which they are getting until the end of the trial. And even when the drug does not help, these data still show how people respond on average.
Understanding averages
Let's look at two examples of randomized, placebo-controlled, blinded clinical trials with dopaminergic drugs, specifically one each studying a dopamine agonist and then levodopa.
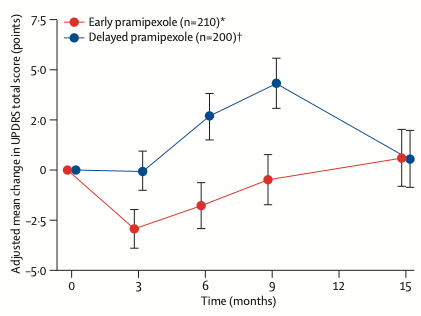
Let's consider how to interpret the results of a study by Schapira et al with a dopamine agonist that was published in Lancet Neurology in 2013. This trial enrolled over 500 people with early PD using a delayed-start design. This type of trial is useful when the therapy being tested is known to improve symptoms when it is started. The people who are randomly chosen to receive placebo at the beginning get the active drug after 6-9 months to see if they "catch up" to the group that started with the active drug. If they do catch up, this means that the drug is not affecting the underlying disease, although it does affect symptoms.
The graph below show data from Schapira et al shows how people respond on average. The graph has the change in total UPDRS score on the y-axis and time in months on the x-axis, which extends to 15 months. a negative number means symptoms of PD are reduced. The group labeled "early pramipexole" (in red) are people randomly chosen to get the active drug immediately, whereas the "delayed pramipexole" group (in blue) started with placebo and then at month 9 were given active drug.
This dopamine agonist "works" to reduce symptom severity by the 3rd month of taking the medicine. But on average, that benefit starts to go away by the 6th month of treatment (red line). The effect of the drug is better than placebo - it does work - but the benefit that people feel initially is almost gone by the 9th month of taking the medicine. And those started on placebo that switched to active drug at 9 months improved to a level as good as those who started the medicine immediately.
So you may have a different experience with symptoms of PD depending on whether starting the drug immediately or 9 months later, but you end up in the same spot after 15 months with either choice.
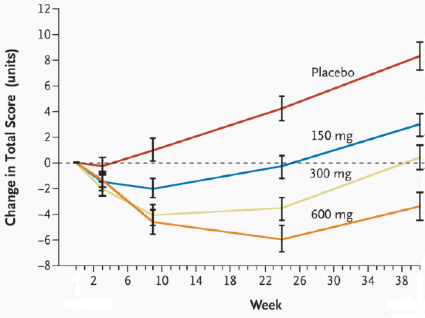
It's a similar story for levodopa, as shown by these data from the ELLDOPA study published in the New England Journal of Medicine in 2004. Whether treated with 150 (blue), 300 (yellow) or 600 mg (orange) daily, symptoms improved by week 3 and were even better after 9 weeks of treatment. But for those treated with 150 mg or 300 mg of levodopa daily, the benefit was starting to wear off by 24 weeks of treatment, at which time the benefit of the lowest dose had already worn off. And by 40 weeks, the benefit of the 300 mg dose also had worn off. Treatment with levodopa made people feel better than those people given a placebo, but unfortunately, any improvement with levodopa was wearing off or already gone well before 40 weeks. Again, this is not much of a success story.
Planning for your future
Once we understand the average response to treatment, there are some really difficult issues that follow. How does one plan for work/career? How can one prepare for retirement? How does one decide what to do - and when - with family and friends?
For many of us, denial can be a useful coping mechanism. "If I can manage today, then why should I worry about the future?" For others, there can be a "bucket-list" approach of traveling, learning new skills or spending time with loved ones.
While planning is hard to get perfect based on the variability in how the disease affects individuals differently, the averages show the importance of planning. If you are having trouble walking and moving, and your doctor suggests taking a new drug, perhaps that trip to visit your grandchildren should be 3-4 months after starting rather than in 6-9 months. And then there can be the challenge of managing work. Does it make sense to speak with an attorney to find out if you can be protected due to your PD qualifying as a disability?
No one can tell you how to plan for life with a disease like Parkinson's, but there are advantages for those who do plan. I urge you to do so, based on how averages can show you the likelier effects of the disease.
Share This
|
Sign up at: ParkinsonsDisease.blog |
About Jonathan Sackner-Bernstein, MD
Dr. Sackner-Bernstein shares his pursuit of conquering Parkinson's, using expertise developed as Columbia University faculty, FDA senior official, DARPA insider and witness to the toll of PD.
Dr. S-B’s Linkedin page
RightBrainBio, Inc. was incorporated in 2022 to develope dopamine reduction therapy for people with Parkinson's.