Breaking news... an important Parkinson's discovery
Forgive my sensationalism, as this is not a new discovery in the traditional sense.
There are no new clinical trial findings. In fact, there are no new data. Instead, we asked a question about dyskinesias a bit differently than is conventional. By doing so, we learned something new about dyskinesia.
Dyskinesia refers to uncontrollable, abnormal movements. And when people with Parkinson's develop dyskinesia, it can be pretty shocking. I'm not talking about a tremor, which is classically a rhythmic movement of a hand or fingers. I'm referring to spasms that can affect almost any part of the body, ranging from facial tics to unpredictable arm swinging. In the standard questionnaire used to assess clinical condition in PD (UPDRS), dyskinesia is described as wiggling, twitching or irregular jerking.
Don't click on this video. Yet.
This video is only 2 minutes long. But it only takes 20 seconds until Matt's dyskinesia is evident. And by 30 seconds, it's pretty upsetting to see how dyskinesia can affect someone with Parkinson's. In fact, I'm not sure I could watch this whole thing if I had Parkinson's. Okay, those of you willing to watch a graphic example of pretty severe dyskinesia can watch now.
The cause of dyskinesia is unknown. The standard teaching is that dyskinesia is related to use of levodopa therapy in advanced cases of Parkinson's. The movements get worse and are caused by peak levels of dopamine getting too high. In that context, delivery methods have been developed to keep blood levels of dopamine (and therefore brain levels) from getting too high or too low.
The graph below from the study by Othman shows blood levels of levodopa when patients with advanced Parkinson's area treated with either intestinal infusion (DuopaTM) via a pump or pills taken by mouth. You can see the way levodopa levels hit peaks and valleys when taking pills (in red) and how the intestinal infusion keeps levels constant all day (12 hours).
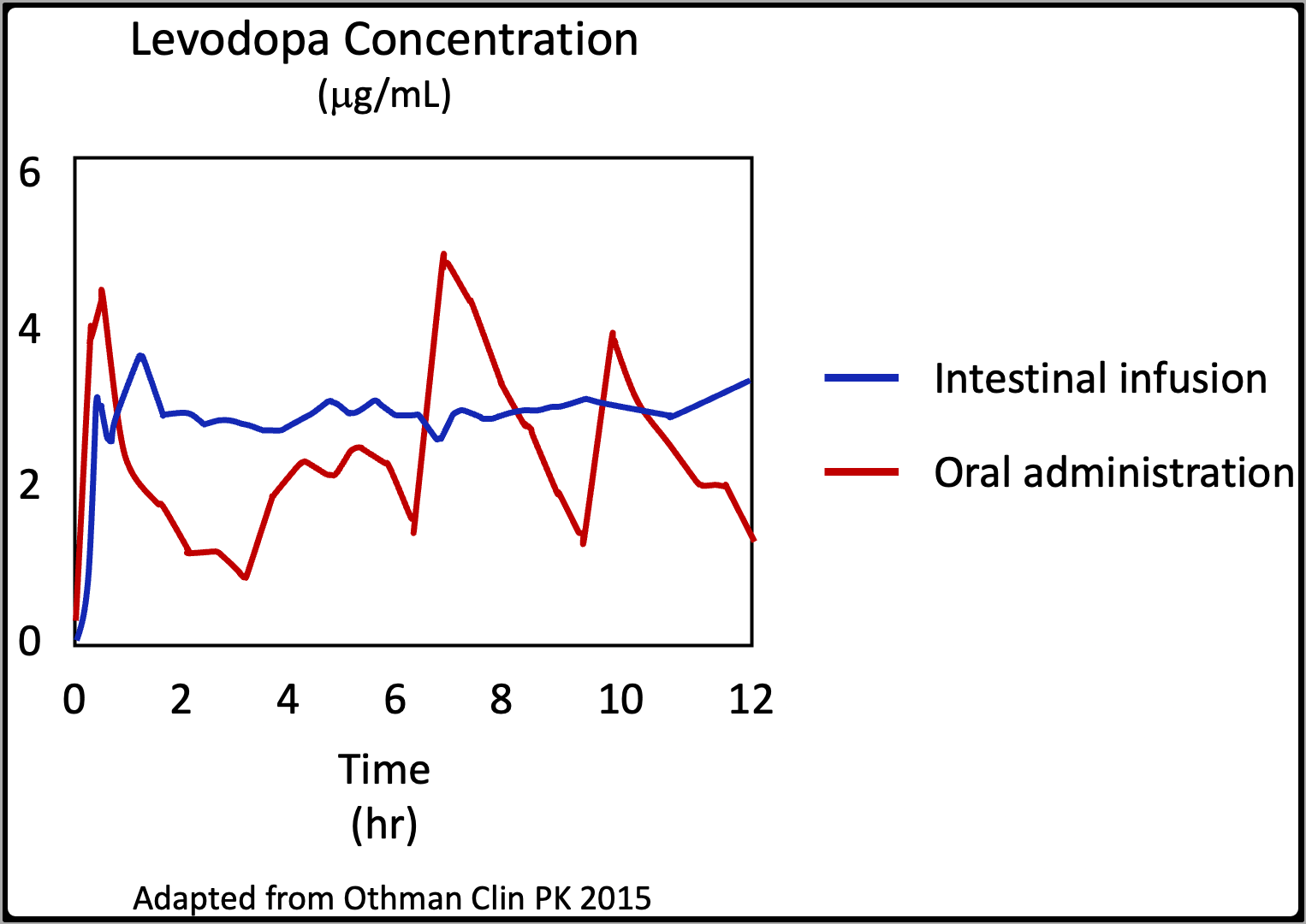
If dyskinesia were caused by peaks in drug levels, then these data suggest that intestinal infusion of levodopa should eliminate dyskinesia. The same argument could be made about a new version of levodopa that is pumped under the skin as a constant infusion.
There is one randomized, double-blind trial of intestinal infusion compared to oral levodopa (Olanow et al, Lancet Neurology, 2014). Abbvie (the Sponsor) provided these summary data, which is pretty dense, so let me explain what the study showed.
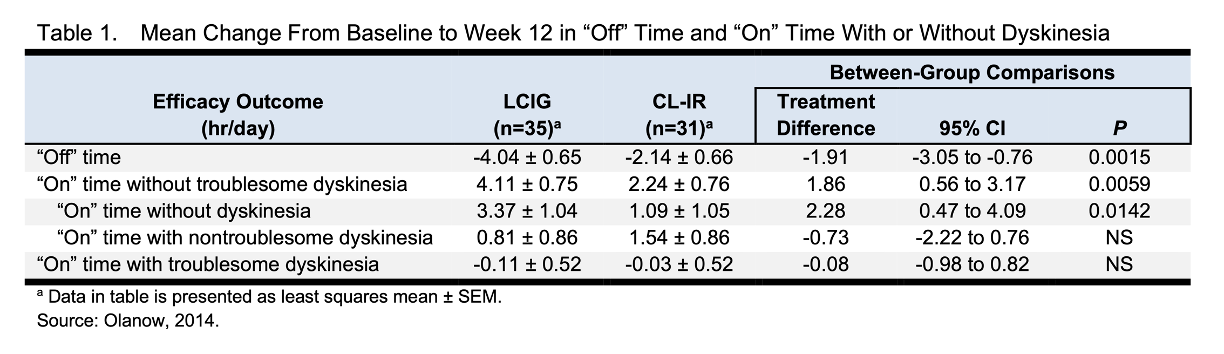
First question: does avoiding the peaks and valleys in drug levels get rid of dyskinesia? Answer: no.
Second question: does avoiding the peaks and valleys in drug levels help with dyskinesia? Answer: yes.
You can see in this table how either approach impacts dyskinesia. Remember, if the cause is peak levels getting too high, we'd expect dyskinesia to go away when teh peaks and valleys in drug level go away. But dyskinesia does not go away with constant levels. Look at the column marked "LCIG" (abbreviation for Levodopa-Carbidopa Intestinal Gel). Constant level therapy reduces any dyskinesia by about 2.25 hours better than pills ("on" time without dyskinesia). And constant level therapy reduces troublesome dyskinesia ("on" time with troublesome dyskinesia) by a bit more than 1.75 hours. These are important benefits of levodopa treatment delivered at constant levels.
But constant therapy that eliminates high peak levels does not "fix" dyskinesia. In people who start out moving well without dyskinesia an average of 6.3 hours a day, which means they are not moving well and/or suffering from dyskinesia almost 18 hours a day. Constant dopamine infusion reduces that to moving well without any dyskinesia an average of 2.9 hours a day. And when looking at the data for moving well without "troublesome" dyskinesia, the improvement is from 8.7 to 4.3 hours a day. These are important improvements, especially when considering how disabling bad dyskinesia can be. Just ask Matt in the video above. But the use of pumps to deliver constant infusions instead of pills does not get rid of dyskinesia.
This is the breakthrough I was referring to in the title. Dyskinesia in people with Parkinson's is not caused by excessively high peak levels.
Do such peak levels contribute? Probably, but we can't kid ourselves. There are no data showing that avoiding the peaks and valleys fixes the problem, so based on available data, we cannot conclude that the peaks and valleys are the cause.
We need to stop spending time, money and energy - and giving people false hope - that use of catheters, tubes and pumps will fix this terrible problem. As with dopaminergic therapies in general, I believe the data are pretty clear. These are all important, high impact therapies - but for palliation and not to address the underlying cause(s) of the disease.
How many lessons do we need before we realize that the currently accepted models of Parkinson's disease will not lead to a therapy that conquers the disease?
Share This|
Sign up at: ParkinsonsDisease.blog |
About Jonathan Sackner-Bernstein, MD
Dr. Sackner-Bernstein shares his pursuit of conquering Parkinson's, using expertise developed as Columbia University faculty, FDA senior official, DARPA insider and witness to the toll of PD.
Dr. S-B’s Linkedin page
RightBrainBio, Inc. was incorporated in 2022 to develope dopamine reduction therapy for people with Parkinson's.